What is intrauterine insemination, how it works, and its advantages

Intrauterine insemination (IUI) is a fertility treatment that helps increase the chances of pregnancy. It consists of placing a prepared semen sample directly inside the uterus at the exact moment of ovulation to make it easier for sperm to reach the egg.
It is a quick, outpatient, and practically painless procedure, ideal in cases such as mild male infertility, ovulation problems, unexplained infertility, the use of donor sperm, or as an alternative before in vitro fertilization (IVF). In this blog, we explain what intrauterine insemination is, how it works step-by-step, and when it is recommended.
What is intrauterine insemination (IUI)?
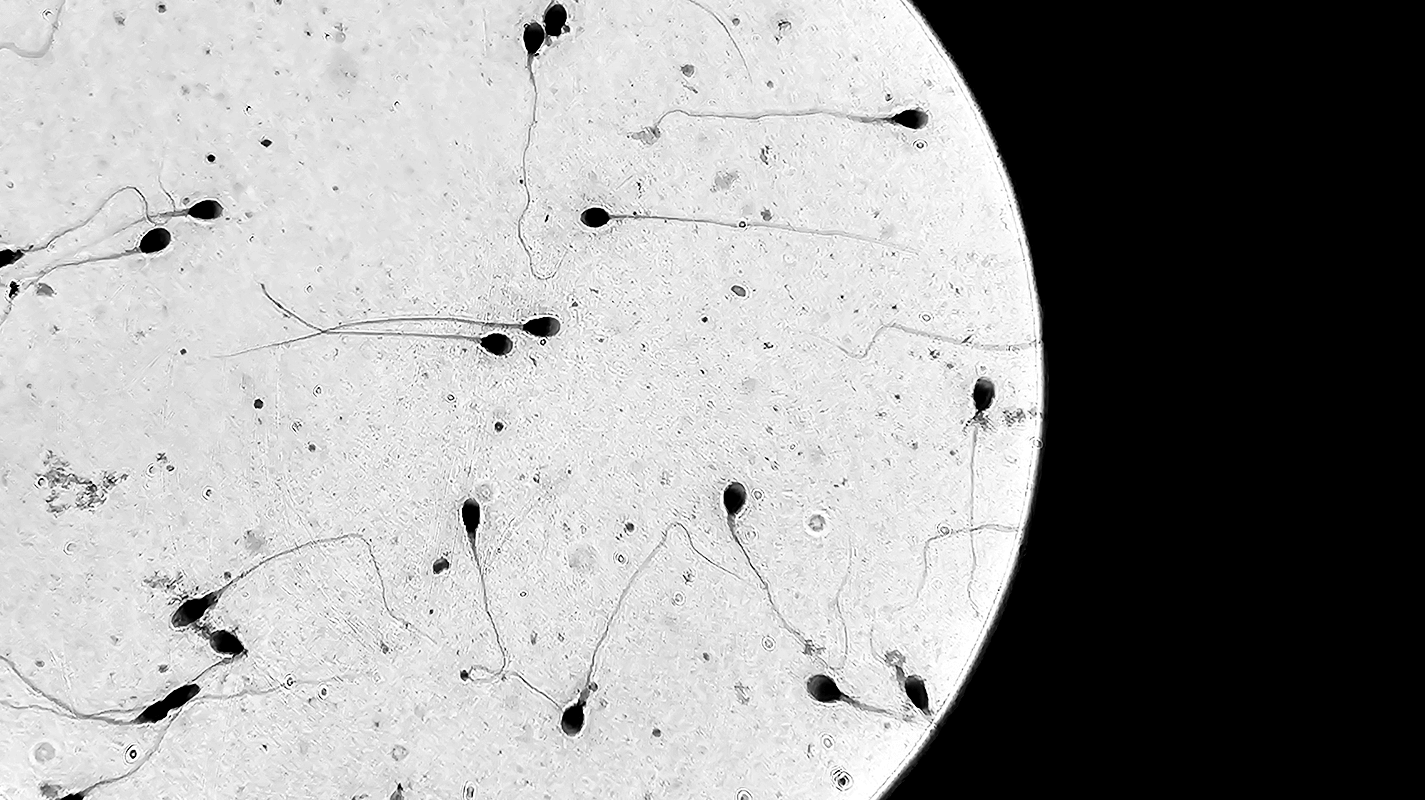
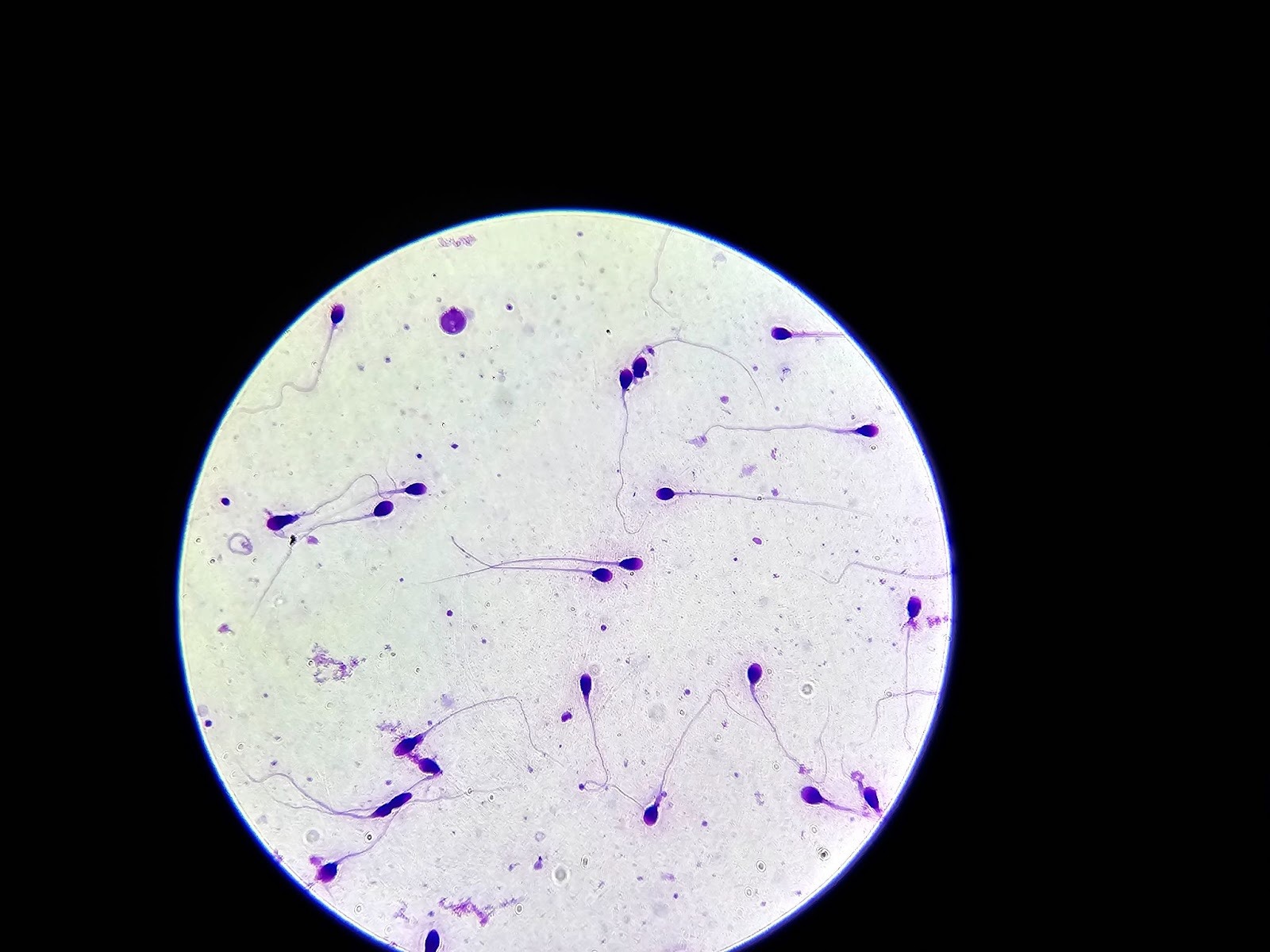
Intrauterine insemination is an assisted reproductive technique in which a semen sample (from a partner or donor) is processed in the laboratory to select the highest-quality motile sperm, which are then deposited in a controlled manner inside the woman’s uterus. To reach that point, the catheter passes through the cervix, placing the sample closer to the fallopian tubes, where fertilization naturally occurs. This technique is part of first-line treatments before resorting to more complex procedures such as in vitro fertilization (IVF).
In a menstrual cycle without intervention, sperm must overcome multiple barriers: the vaginal environment, cervical mucus, the cervix, the uterine cavity, and finally reach the fallopian tubes. When there is a mild infertility factor, whether due to semen abnormalities (male factor), ovulatory disturbances, or issues with the cervical environment, this journey may be compromised. The goal of intrauterine insemination is to reduce these barriers and facilitate the path.
Although it is often referred to as “artificial insemination,” at Fertilidad Integral we consider it important to clarify this term. The word artificial refers only to the fact that the process is aided by science and reproductive medicine, it does not mean that the pregnancy is “less natural” or “less real.” Bodies that require support to conceive are not less valuable, and pregnancies achieved through fertility treatments, such as intrauterine insemination or in vitro fertilization, are just as legitimate, desired, and deeply human.
Artificial insemination is not artificial
In everyday language, the word “artificial” is often associated with something fake or lower quality. In medicine and particularly in obstetrics and gynecology, the term is used differently: it simply indicates that a process was assisted by humans rather than occurring spontaneously.
In any type of artificial insemination, including intrauterine insemination, science allows us to place sperm at a precise point in the female reproductive tract, optimizing timing and location. Fertilization, however, still occurs in the fallopian tubes, inside the patient’s body, guided by the same biological mechanisms as in a spontaneous pregnancy.
At Fertilidad Integral, we highlight that:
- “Artificial” does not mean worse or less valid.
- People with fertility challenges or who are considered subfertile are not less capable or less valuable.
- Pregnancies achieved through reproductive medicine, whether IUI or IVF, are natural pregnancies that develop in the uterus and ideally culminate in a healthy birth.
Technology in this context does not replace the body; it supports and enhances it.

How does intrauterine insemination work?
The functioning of intrauterine insemination is based on two principles:
- Synchronizing the moment of ovulation with the placement of a high-quality semen sample.
- Reducing the distance sperm must travel to reach the egg.
To better understand the procedure, it is useful to divide it into three stages: how you prepare, what happens during the procedure, and what occurs afterward.
How you prepare for an intrauterine insemination
Before recommending intrauterine insemination, a reproductive medicine specialist evaluates several factors:
- Menstrual cycle and ovulation: whether the patient ovulates regularly, how the follicular and luteal phases behave, and whether there are ovulatory disorders.
- Ultrasound: to assess follicular development and uterine structure.
- Laboratory tests: including antimüllerian hormone (AMH), allowing assessment of ovarian reserve and reproductive potential.
- Semen analysis: to evaluate sperm count, motility, morphology, and other male-factor variables.
With this information, the physician determines whether IUI is the appropriate treatment or whether another approach, such as IVF, is more suitable.
During this stage, we study, prepare, and monitor your menstrual cycle, whether through medication, ovulation prediction kits, ultrasound imaging, or hormonal testing to evaluate follicular development and hormone levels. Our goal is to ensure optimal preparation to begin your fertility treatment with precision and support.
During the procedure for an intrauterine insemination
On the chosen day for insemination, the semen sample is obtained, either from the partner or from a donor.
The procedure is outpatient and usually lasts only a few minutes:
- The patient lies in a gynecological position.
- The physician inserts a speculum to visualize the cervix.
- A soft, very thin catheter is passed through the cervix into the uterine cavity.
- The prepared semen sample is slowly deposited.
This procedure is performed in the clinic’s examination rooms and does not require surgery.
After the procedure for an intrauterine insemination
From that point:
- Sperm begin their journey toward the fallopian tubes to meet the egg.
- If fertilization occurs, the embryo travels back to the uterus and attempts to implant in the endometrium during the luteal phase.
- Implantation typically occurs 6–10 days after the procedure.
Two weeks later, you can take a pregnancy test to measure hCG.
Who is a good candidate for intrauterine insemination?
Not everyone with fertility challenges is a candidate for IUI. Proper selection is key for success.
Good candidates include:
- Mild to moderate male factor infertility, where sperm count or motility is moderately reduced but still sufficient for processing.
- Mild ovulatory disorders, such as irregular cycles, occasional anovulation, or controlled polycystic ovary syndrome.
- Unexplained infertility, when no clear cause is identified despite a complete evaluation.
- Cervical mucus or cervical factor abnormalities that hinder sperm transport.
- Couples with difficulty timing intercourse due to pain, vaginismus, physical limitations, or logistical barriers.
- Single mothers by choice or same-sex female couples using donor sperm.
- Mild endometriosis, when the rest of the evaluation is favorable.
In general, the highest success rates occur in younger women with good ovarian reserve, permeable fallopian tubes, and non-severe male factor.
Who is not a candidate for intrauterine insemination?
IUI is usually not appropriate in cases of:
- Blocked or severely damaged fallopian tubes, since fertilization occurs there.
- Severe male factor infertility, where IVF with ICSI offers better success.
- Very low ovarian reserve, where egg quality is significantly diminished.
- Hostile or inadequate uterine cavity, where anatomical or functional conditions do not favor implantation.
In these scenarios, other fertility treatments, such as IVF, are generally recommended.
Types of intrauterine insemination
Partner sperm
Used when a heterosexual couple has mild to moderate male factor infertility, or even normal semen, but remains subfertile.
The sample is obtained the same day, processed in the lab, and concentrated into a small volume placed inside the uterus to increase the number of sperm reaching the egg.
Donor sperm
Used in cases of severe male factor infertility, absence of sperm in the ejaculate, high-risk genetic conditions, same-sex female couples, or single mothers by choice. Donor sperm comes from certified sperm banks.
The procedure is the same; only the origin of the sample changes.
Intrauterine insemination vs. other treatments
IUI is one option within the spectrum of reproductive medicine. It is neither better nor worse, it is simply more appropriate for certain patients.
Intrauterine insemination vs. in vitro fertilization
IVF is a technique in which fertilization occurs in the laboratory rather than in the fallopian tubes. It requires stronger ovarian stimulation, egg retrieval through an outpatient procedure, and later embryo transfer.
IUI is often recommended as a first-line treatment in good-prognosis cases; IVF is typically reserved for more complex scenarios or when simpler treatments have not worked.
Intrauterine insemination vs. timed intercourse
Timed intercourse involves monitoring the menstrual cycle, identifying ovulation via ultrasound or hormonal tests, and recommending intercourse on the most fertile days.
Timed intercourse can be helpful as a first step in young couples without clear infertility problems. When success probabilities are lower or search time is prolonged, IUI offers better control and higher pregnancy rates.
How much does intrauterine insemination cost in Mexico?
At Fertilidad Integral, IUI starts at $17,000 MXN without medication (approx. $923 USD). This includes the insemination procedure, semen preparation, and care in a specialized reproductive setting.
What’s included?
- Dedicated care team
- Cycle monitoring via ultrasound and hormone testing
- Ovulation induction medication
- Semen collection and preparation
- Insemination performed with a thin catheter
- Follow-up consultation
The medications are not included. The average cost of ovarian stimulation and hormonal support medications is approximately $7,000 MXN, although this may vary depending on the clinical case, diagnosis, and ovarian response. On average, the additional investment can range between $5,000 and $15,000 MXN.
There may be additional costs for prior diagnostic studies, depending on the clinical case, as well as sperm bank fees if donor sperm is required.
In the United States, costs can vary widely depending on the state, insurance coverage, and type of clinic. Without insurance, the basic intrauterine insemination procedure typically costs between $300 and $1,000 USD, but once medications, diagnostic tests, and sperm processing are added, the total cost can increase up to $4,000 USD per cycle. At Fertilidad Integral, it is significantly more accessible without sacrificing quality standards.
Why choose Fertilidad Integral?
Fertilidad Integral is a clinic specialized in fertility and preservation treatments. With cutting-edge technology and a human-centered perspective, it transforms the way fertility is understood and treated.
Some key differentiators include:
A holistic approach
We understand the body as a connected system. That’s why we work with psychology, nutrition, acupuncture, and massage therapy, integrating each specialty so that your process feels fully supported from every angle.
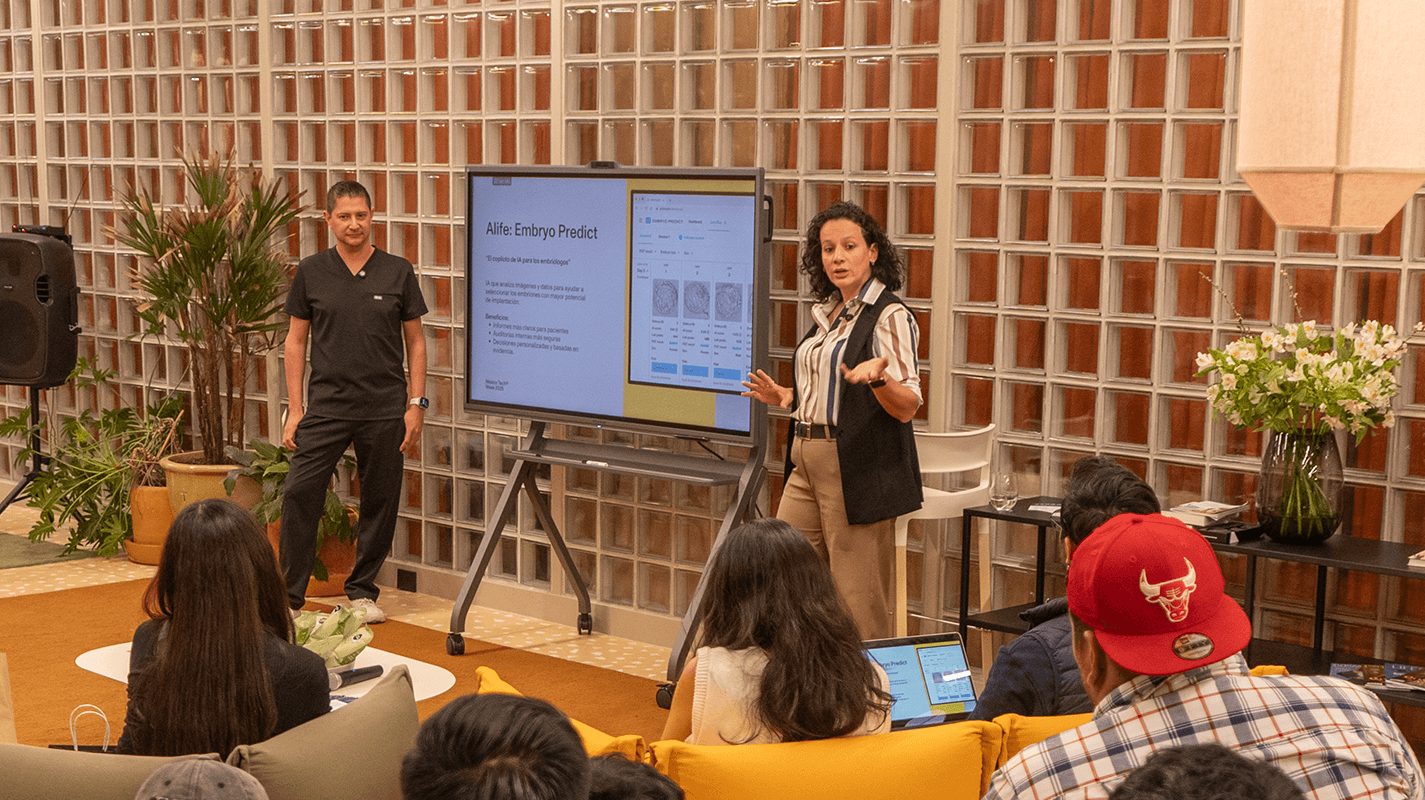
Advanced technology and certified specialists by your side
We have a laboratory equipped with state-of-the-art systems, safety protocols such as RI Witness, and artificial intelligence tools like Alife Health, supported by a team of certified physicians and embryologists who are leaders in reproductive medicine.
Personalized treatment plans in conception and preservation
We design individualized plans based on each patient’s medical history, ovarian reserve, male factor evaluation, and reproductive goals, optimizing every step of the process to achieve the best possible outcomes.

Frequently asked questions about intrauterine insemination
How effective is intrauterine insemination?
Effectiveness depends mainly on the woman’s age, the cause of infertility, and the quality of the semen sample. In general, pregnancy rates per cycle range between 10–20% in good-prognosis patients and may improve when several treatment cycles are combined.
What are the chances of pregnancy with intrauterine insemination?
Chances usually range between 10–15% per cycle in low-complexity treatments and can reach 27–47% when multiple cycles are considered in young patients with good ovarian reserve, open fallopian tubes, and favorable male factor. The cumulative success rate increases with consecutive cycles when the indication is appropriate.
How many women get pregnant on the first insemination?
A proportion of patients achieve pregnancy on the first attempt; however, probabilities are generally calculated cumulatively. In practice, many guidelines recommend considering three to four cycles of intrauterine insemination before deciding whether to continue or switch to another technique, such as in vitro fertilization.
How many days after intrauterine insemination does implantation occur?
If fertilization occurs successfully, the embryo travels through the fallopian tube into the uterus, and implantation typically takes place between 6 and 10 days after insemination. Confirmation is performed via a blood pregnancy test approximately 12–14 days after the procedure.
How many times can a person undergo intrauterine insemination treatment?
There is no strict limit, but generally, three to four cycles are recommended for couples with good prognosis. If pregnancy is not achieved after that number of attempts, at Fertilidad Integral we assess whether the expected success rate remains reasonable or if it is more appropriate to move toward in vitro fertilization (IVF) or another strategy.
What are the risks or side effects of intrauterine insemination?
IUI is a safe procedure, but like any medical intervention, it is not free of risks:
- Mild discomfort or transient cramping during or after the procedure.
- Slight vaginal spotting afterward, usually self-limited.
- Very low risk of pelvic infection.
- Risk of multiple pregnancy when combined with ovarian stimulation, especially if several follicles develop; this risk is reduced with careful monitoring.
What are the chances of a multiple pregnancy with intrauterine insemination?
The risk of multiple pregnancy is higher than in a completely spontaneous cycle, especially when ovarian stimulation is used. However, with adequate protocols, the goal is to promote the development of only one or, at most, two dominant follicles.
Your fertility, at your own pace
The decision to begin a fertility treatment is deeply personal. Understanding what intrauterine insemination is, how it works, and in which cases it offers the best chances of success can help you make informed decisions about your reproductive health.
If you want to know whether intrauterine insemination is right for you, or what other assisted reproduction alternatives you might consider, at Fertilidad Integral we can help you review your medical history, your results, and your goals.
Schedule your fertility check-up to receive a personalized evaluation and discover, with clarity and professional support, the options available for your case.